John Grigg
Senior Lecturer
Department of Ophthalmology, University of Sydney
[email protected]
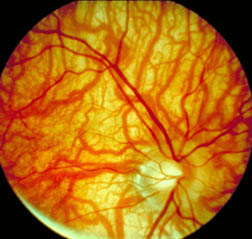
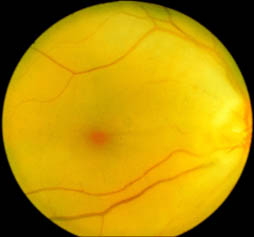
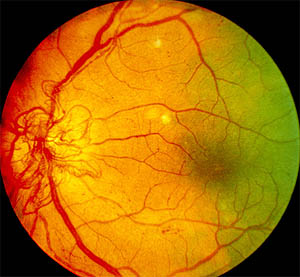
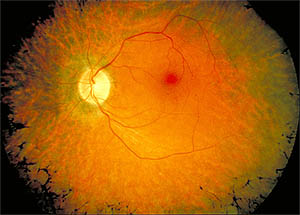
- Right Fundus
- Posterior Pole
Clinical Facts
- Optic disc with small central cup and peri-disc atrophy
- Oval macula with central fovea
- Retinal vessels
- Veins deeper red and thicker
- Arteries lighter red and thinner calibre
- Note how vessels form 4 main arcades (superior temporal, Superior nasal, inferior temporal and Inferior nasal) - Note: Vertical dark central line ending on fovea is internal camera fixation device.
Learning Topics
- How do you identify the eye from a photo of the posterior pole?
- What are the dimensions of the optic disc and macula?
- Why are there no blood vessels in the centre of the macular?

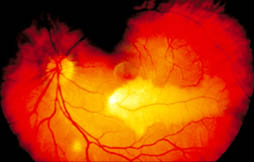
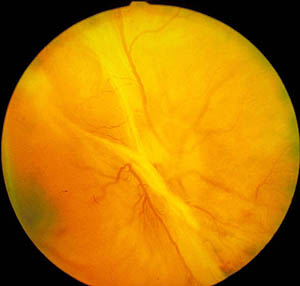
Clinical Description
- Minimal Retinal and Choroidal pigment
- Easy visualisation of choroidal vessels
- Note: poor delineation of macula
Clinical Facts
- Albinism can be isolated ocular anomaly or more commonly part of a systemic syndrome
- Fundi with little pigment also occur in people with myope
Learning Topics
- Be able to differentiate a choroidal vessel compared to retinal vessel
- If a person had normal pigmentation but choroidal vessels were visible, what disease process could be present to explain this?
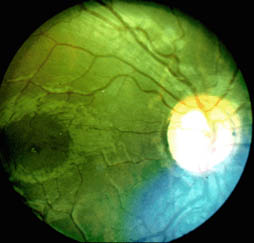
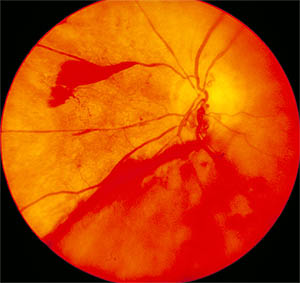
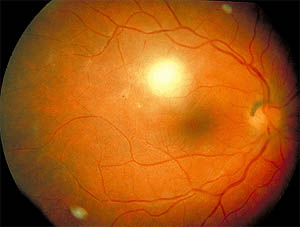
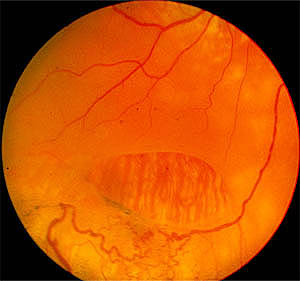
Clinical Description
- Infero-temporal retinal oedema
- Note embolus in infero-temporal artery
Learning Topics
- For the patient in this slide what do you think their visual acuity would be and why?
- Following a retinal embolus
- what is the risk of a myocardial infraction over 5 years?
- what is the risk of death in the next 5 years?
- what is the risk of a completed stroke over 1 year?
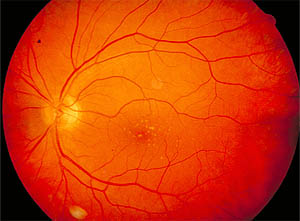
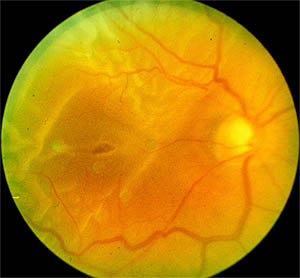
Clinical Description
- Heavily pigmented fundus in dark skinned people
- Note: no choroidal vascular pattern seen
Learning Topics
The red reflex may not be red
- What are some causes which are due to pathology and what are the other colours?
- What are causes for a different coloured red reflex when there is no pathology?
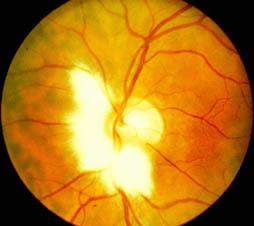
Clinical Description
- White fluffy edged patch overlying and covering retinal blood vessels
- Usually adjacent to the optic disc but can occur at other sites along the nerve fibre layer
Clinical Facts
- Extension of myelin onto retina
- May be a cause of pseudopapilledema
Learning Topics
- Where does normal myelination end?
- What is the pattern of the nerve fibre layer?
Clinical Description
- Irregular, "lumpy" disc margin, due to hyalin-like calcific material within the substance of the optic disc
Clinical Facts
- 0.3% of population
- Autosomal Dominant inheritance in some cases
- In children, deposits lie deep in disc substance resulting in appearance of a swollen disc
Learning Topics
- How could you tell this appearance from true papilledema?
- What would a CT Scan show?
- What would an ultrasound examination of the eye show?

Clinical Description
- Area of peripapillary atrophy
- Note size of optic disc (do not confuse with boundaries of atrophy)
- Optic disc is often larger in a person with myopia compared to Hypermetropia
Clinical Facts
- Degenerative myopia (Refractive error greater than 6 diopters)
- Due to poorly understood pathogenic mechanism which results in progressive elongation of the globe.
- The complications of myopia are a common cause of visual loss list 2 causes

Clinical Description
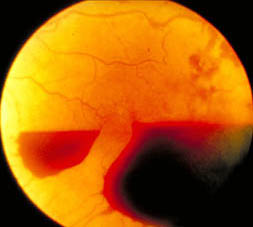
- The blood lies between the posterior face of the vitreous and the retina
- Note how the blood obscures the retinal vessels helping to indicate the anatomic layer involved by the pathologic process
Learning Topics
- What condition is likely to be associated with this type of haemorrhage and why?
Clinical Description
- Copper wiring of arteries/arterioles
- Arterio-venous nipping
- Arteriolar narrowing approximately 1/3 of vein diameter
Clinical Facts
- Hypertensive Retinopathy
- Severity: reflected by the degree of hypertensive vascular changes and retinopathy
- Duration: is reflected by the degree of arteriosclerotic vascular changes and retinopathy
- Hypertensive Vascular Changes
- Vasoconstriction and leakage principal clinical signs
- Width of artery normally 2/3 - 3/4 size of vein
• GRADE 1
- Mild generalised arteriolar attenuation
- Approx 1/2 calibre of veins
- Difficult to tell
• GRADE 2
- Grade 1 + focal arteriolar attenuation
- 1/3 calibre of vein
• GRADE 3
- grade 2 + haemorrhages, cotton wool spots and exudates
• GRADE 4
- (Malignant Hypertensive retinopathy) Grade 3 + disc swelling
- Arteriosclerotic Features
- Arteriovenous (AV) crossing changes are most important sign
• GRADE 1
- Broadening of arteriolar light reflex
- Can be difficult to determine
• GRADE 2
- Grade 1 + deflection of veins at A-V crossings (Salus' sign)
• GRADE 3
- Grade 2 + "copper-wire" arterioles and marked AV crossing changes
- Tapering of the vein on either side of the crossing, right hand bends in veins at crossings
• GRADE 4
- Grade 3 + "silver wire" and severe AV crossing changes which may be associated with branch retinal vein occlusions

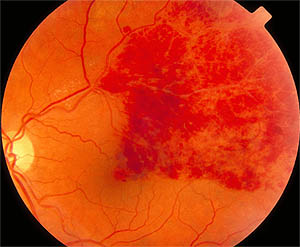
Clinical Description
- Cotton wool spots (soft exudates)
- Hard exudates with arrangement into macular star
- Flame shaped haemorrhages (Nerve fibre layer)
Learning Topics
- What is a systemic hypertensive condition associated with accelerated hypertensive retinopathy?
- What is the age when it most commonly affects individuals?

Clinical Description
- Pale swollen (oedematous) retina
- Cherry red spot at the macula
- Attenuated arteries
Learning Topics
- Describe the appearance of the optic nerve in central retinal artery Occlusion
- Why does the macula appear red (cherry red spot)?
- What are common causes of CRAO?
- What are the symptoms that the patient is likely to describe?
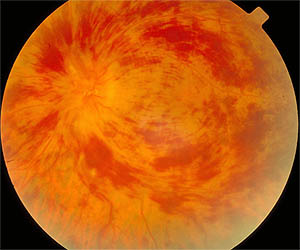
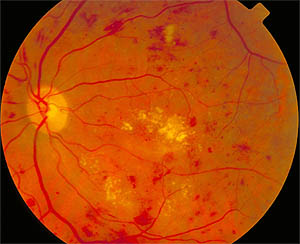
Clinical Description
- Dilated tortuous retinal veins
- Multiple retinal haemorrhages (dot, blot & flame-shaped)
- Typical Cases haemorrhages moderate number and most numerous in the peripheral retina - Swollen disc mild to moderate
- Rare cotton wool spots
- Mild-moderate macular oedema
Clinical Facts
- Visual acuity usually better than 6/60
- 50% of cases resolve spontaneously and visual acuity returns to near normal
Learning Topics
- List several systemic conditions associated with CRVO
- Discuss investigational workup for these patients
- Why is this sometimes called "a red infarct"?
Clinical Description
- Numerous cotton wool spots
- Haemorrhages can affect posterior pole equally as periphery
- Macula markedly oedematous
- Marked optic disc swelling
Clinical Facts
- Poor vision - usually less than 6/60
- Relative afferent pupil defect present
- Complications of retinal ischaemia include
- retinal neovascularisation
- iris neovascularization
- These can be complicated by vitreous haemorrhage and glaucoma

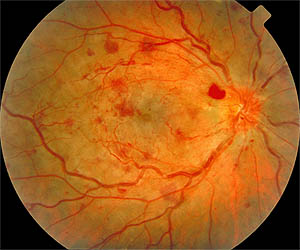
Clinical Description
- Haemorrhage and retinal oedema occur only peripheral to the site of the occlusion
Clinical Facts
- Visual outcome is dependent on the site of the occlusion i.e. macular branch vein and the amount of venous drainage involved
- The larger the area involved the greater the chance for permanent Ischaemia
- Ischaemic retina produces cyto-lines that stimulate neovascularisation, which in the eye are frequently complicated by haemorrhage, tractional retinal detachment and glaucoma
- Risk of neovascularisation greatest for those with a retinal area of ischaemia greater than or equal to 5 disc diameters in diameter
- These patients should have prophylactic laser photocoagulation to the ischaemic area
Clinical Description
- Note tortuous venous shunt vessels on the optic disc
- Residual retinal haemorrhages
Clinical Facts
Other features that indicate chronicity
- Venous sheathing
- Chronic cystoid macular oedema
- Shunt vessels
- Collaterals
- Cholesterol crystals from chronic exudation
Collaterals
- Are pre-existing retinal capillaries that bypass adjacent areas of vascular closureShunts
- Are arteriovenous communications that bypass capillary beds

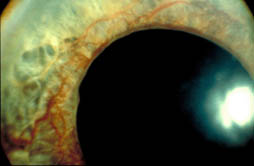
Clinical Description
- Dilated new vessels on the iris surface
Clinical Facts
- These new vessels often occur in the anterior chamber angle
Learning Topics
- What are the complications of rubeosis iridis?
- What conditions cause rubeosis iridis?
Clinical Description
- DOT haemorrhages - represent microaneurysms
- Flame shaped haemorrhages (nerve fibre layer haemorrhages)
- Blot haemorrhages
- Hard Exudates
Learning Topics
- Clinical signs that divide diabetic retinopathy (DR) into background DR, pre-proliferative DR, proliferative DR and diabetic maculopathy

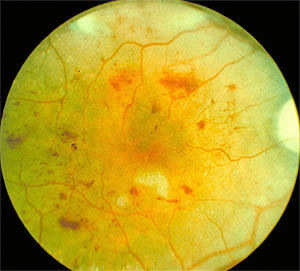
Clinical Description
- Blot haemorrhages
- Cotton wool spots
Clinical Facts
In addition to the features of background diabetic retinopathy there are the followings signs: - Cotton wool spots
- Venous changes including dilation, beading & sausage like segmentation
- Intraretinal microvascular abnormalities (IRMA). These are focal areas of flat retinal malformations which DO NOT leak on fluorescein angiography
- Large dark blot haemorrhages
- If there is significant areas of retinal ischaemia then laser photocoagulation therapy is appropriate to the ischaemic areas
Learning Topics
- Does diabetic control alter progression to retinopathy?
- Are there any clinical trials that have addressed this issue?
Clinical Description
- Neovascularisation of the optic disc
- Other diabetic retinopathy signs include:
- cotton wool spots
- dot haemorrhages
Clinical Facts
- New Vessels
- non-fenestrated therefore leak fluorescein
- arise from endothelial proliferations from veins
- Vessels grow in the potential vitreo-retinal space
- Vitreous detachment occurs earlier in diabetic than in people without
Learning Topics
- How do patients lose vision from proliferative diabetic retinopathy?
- Can you prevent or minimise visual loss?
Clinical Description
- Tangential Traction
- Due to contraction of membranes that extend from the posterior retina towards the vitreous base (located just behind the lens zonules and ciliary body). - Bridging Traction
- Due to contraction of membranes that stretch across the posterior retina (behind the glove equator).Learning Topics
- What type of traction is shown in the slide?
Clinical Description
- Blood is seen in the vitreous overlying principally the inferior retina
- Note the irregular outline to the haemorrhage compared to the pre-retinal smooth evescentic outline. These clinical features help to differentiate
Clinical Facts
- Bleeding into the vitreous substance (intragel) can induce syneresis (degeneration with liquification) resulting in further shrinkage of the vitreous, thus allowing traction to occur
with the possibility of tractional retinal detachment
Learning Topics
- What are the principles in managing an acute vitreous haemorrhage?
- Can the blood clear without surgery?
- What is the cup disc ratio in this slide?
- What level is the blood in this fundus?
- What are the possible causes for the haemorrhage?
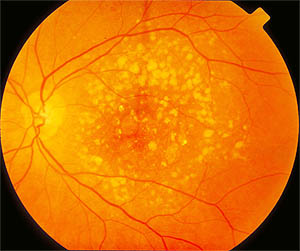
Clinical Description
- Multiple hard drusen in posterior pole
- Note discrete drusen and some confluent drusen
Clinical Facts
- Located between the basal lamina of the RPE and the inner collagenous layer of Bruch's membrane.
- Classified into
- Hard - discrete yellow-white spots
- Soft - indistinct edges
- Calcified - glistening appearance
Learning Topics
- What happens to the retina overlying the drusen with time?
- What is the relationship between drusen and age related macular degeneration?
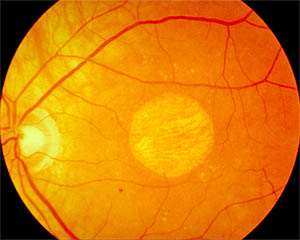
Clinical Description
-
Geographic Atrophy (Non-exudative or dry form)
- Atrophy of retina with surrounding drusen
- Choroidal vessels are seen through the atrophic area
- Note the sharply circumscribed area of atrophy
Clinical Facts
- ARMD is the commonest cause of blindness in the Western World.
- Due to a slowly progressive atrophy of the RPE & photoreceptors.
- Management involves appropriate refraction and good lighting with time magnifying aids and/or large print are provided.
- Continual self monitoring and regular ophthalmic review to check for signs suggesting progression to exudative ARMD.
Clinical Description
- Area of retinal inflammation shown as a white "fluffy" area
- Note: "old" areas of chorioretinitis which are represented as the white
- Flat well circumscribed areas of atrophy
- Note: The clear vitreous
Clinical Facts
- Most common cause of retinitis in non-immunosuppressed person is Toxoplasmosis
- Serology 9is often unreliable
- Toxoplasmosis usually due to reactivation of maternally acquired infection in the Third Trimester. The DDx is AIDS
Learning Topics
- Examine the small vessels supplying the superior macular.
- Are they inflamed?
Clinical Description
- Sharp areas of chorio-retinal atrophy with associated pigment proliferation
- Note: Area of acute inflammation along superior temporal vascular arcade
Learning Topics
- How do people acquire Toxoplasmosis?

Clinical Description
- Bone Spicule pigmentation well demonstrated in inferior fundus
- Attenuated arteries
- Optic disc pallor classically described as waxy
Clinical Facts
Other ocular complications of retinitis pigmentosa: - Cystoid macular Oedema
- Glaucoma
- Cataract
- Myopia
Learning Topics
- What symptoms do RP patients present with?
- Why do they have these symptoms?
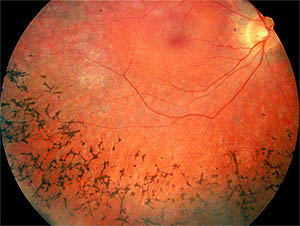
Clinical Description
- Note: Artery calibre compared to the veins
- Note: The bone spicule pigmentation in the periphery
- The choroidal vessels are well visualised out to the pigmentation
Learning Topics
- Why are the Choroidal vessels more prominent?
- Draw the visual field you would expect for this patient
Clinical Description
- Oval shaped retinal hole
- Folded retina on peripheral edge
- Abnormal vascular pattern
Learning Topics
- What symptoms would this patient complain from?
- What are the broad red lines in the base of the hole?
- What is unusual about the vessels at the peripheral area of the tear?
- Draw the retinal and Choroidal vessels and label.
- What pathology can complicate a retinal hole?
Clinical Description
- Crinkled retinal appearance
- Choroidal vessels no longer visible
- Macular detached
Learning Topics
- What symptoms would this patient have?
- How would they differ from a patient with a retinal tear only?
- What would this patient's central vision be?
- What would this patient's peripheral vision be?
Clinical Description