John Grigg
Senior Lecturer
Department of Ophthalmology, University of Sydney
[email protected]
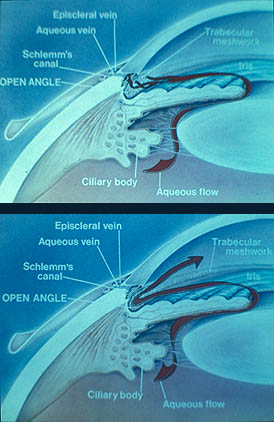
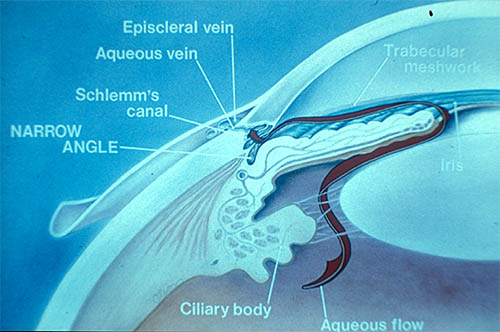
- The vertebrate eye is a fluid filled spheroid having a flexible and partially elastic wall
- maintenance of a stable shape is necessary for optical performance
- IOP = tissue pressure of intraocular contents
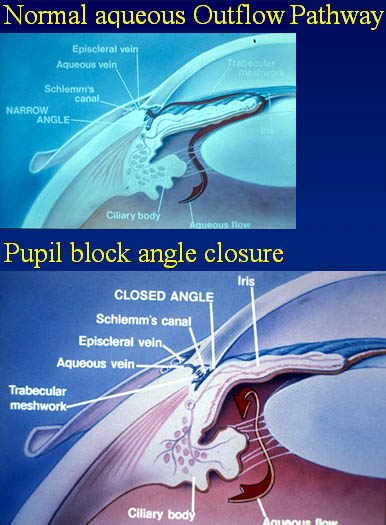
- IOP is maintained in a narrow range by aqueous production matching outflow
|
|
|
|
|
|
- 21 mmHg used as screening pressure not "abnormal" but damage much greater at pressures higher than 21
- chosen because it made search for glaucoma damage more efficient
- Ocular hypertension
- high IOP associated with damage - "Normal tension" glaucoma
- "normal" IOP associated with damage
- Damage
- common with increased IOP
- usually in eye with increased IOP
- asymmetrical IOP
- eg trauma
- truly "low" IOP rare with glaucomatous damage
- Dose response relationship
- IOP 16-19
• risk > 2 times
- IOP > 23
• risk > 10 times
- In population IOP < 22 mmHg is More common than IOP > 22 mmHg
- risk of glaucoma with IOP <22 is approx 1/6 of patients with IOP >22 (2.8 compared to 12.8 see Baltimore Eye study table)
- however, 20 times more people have IOP <22 therefore, adjusted risk of glaucoma is 1:1
- 50% with glaucomatous damage have "normal" IOP
- IOP
- Is associated with nerve damage
- Is a risk factor for nerve damage - IOP is a causal risk factor
- Myopia is associated with POAG
- Myopia is a risk factor for POAG
- It is not a causal risk factor
|
|
Diagrams from "Glaucoma - A Colour Manual of Diagnosis and Treatment" by Jack J. Kanski, James James A. McAllister and John F. Salmon. Butterworth-Heinemann Publishers, a division of Reed Educational & Professional Publishing Ltd
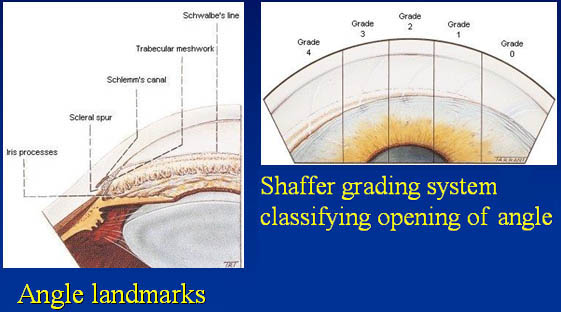
- Ciliary body band:
The most posterior structure appears pink to dull-brown to slate-grey in colour. Its width depends on the position of the iris insertion; tending to be narrower in hypermetropic eyes and wider in myopic eyes. The angle recess represents the dipping of the iris as it inserts into the ciliary body. - Scleral spur:
This is the most anterior projection of the sclera and the site of attachment of the longitudinal muscle of the ciliary body. Gonioscopically, the scleral spur is situated just posterior to the trabeculum and appears as a narrow dense, often shiny, whitish band. It is the most important land-mark because it has a relatively consistent appearance in different eyes. - Trabecular meshwork:
This extends from the scleral spur to Schwalbe's line. The posterior functional pigmented part lies adjacent to the scleral spur and has a greyish-blue translucent appearance. The anterior non-function part lies adjacent to Schwalbe's line and has a whitish colour. Trabecular pigmentation is rare prior to puberty. - Schwalbe's line:
This is the most anterior structure and appears as an opaque line. Anatomically it represents the peripheral termination of Descemet's membrane and the anterior limit of the trabeculum.
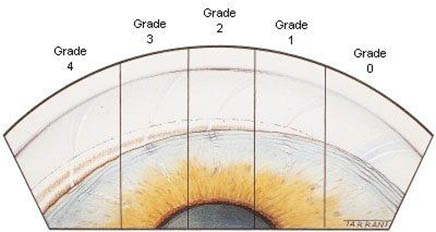
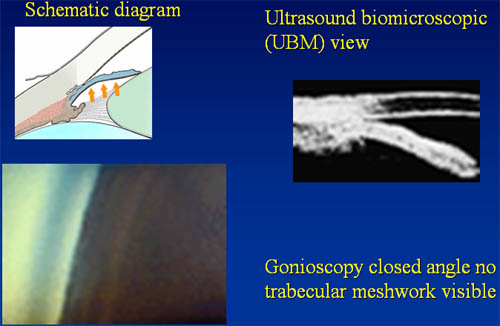
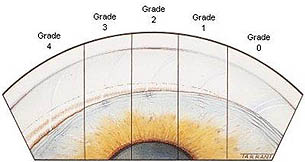
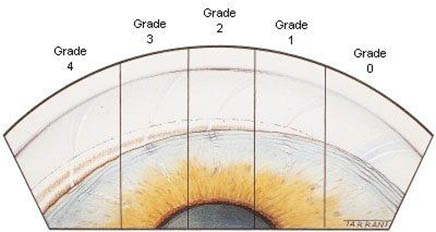
- The examiner grades the angle according to the visibility of the various angle structures.
- Shaffer grading system provides a method of comparing the widths of different chamber angles.
- System assigns a numerical grade to each angle with associated anatomical description, the angle width in degrees and implied clinical interpretation.
|
|
- An "occludable" angle is considered to be an angle in which the pigmented trabecular meshwork is not visible without indentation or manipulation in three quadrants of the circumference.