John Grigg
Senior Lecturer
Department of Ophthalmology, University of Sydney
johng@eye.usyd.edu.au
- Glaucoma is the commonest optic neuropathy
- Diagnosis is made when there is characteristic visual field changes which match the optic disc changes
- The intraocular pressure may be elevated or normal
- Incidence 135,000
- Prevalence 2.9%
Observed prevalence compared to expected age prevalence
- Elderly
- Black race
- Immediate relatives
- Myopic (nearsighted) patients
- Diabetic or hypertensive patients
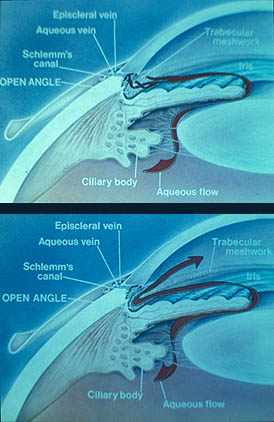
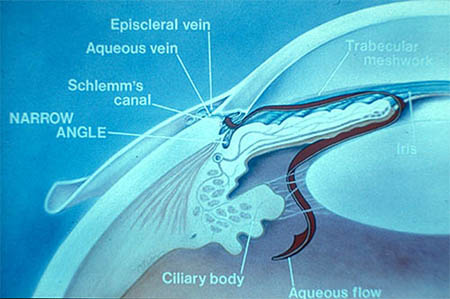
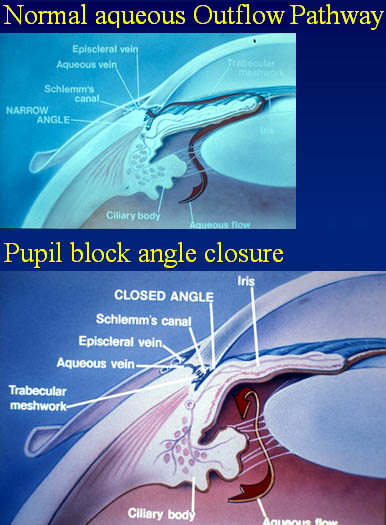
- The vertebrate eye is a fluid filled spheroid having a flexible and partially elastic wall
- maintenance of a stable shape is necessary for optical performance
- IOP = tissue pressure of intraocular contents
- IOP is maintained in a narrow range by aqueous production matching outflow
|
|

|
Schiotz indentation tonometry
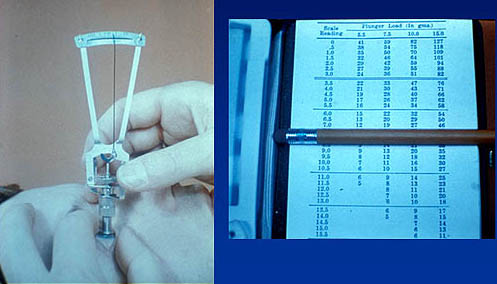
Distribution of IOP
- 21 mmHg used as screening pressure not "abnormal" but damage much greater at pressures higher than 21
- chosen because it made search for glaucoma damage more efficient
- Ocular hypertension
- high IOP associated with damage - "Normal tension" glaucoma
- "normal" IOP associated with damage
- Damage
- common with increased IOP
- usually in eye with increased IOP
- asymmetrical IOP
- eg trauma
- truly "low" IOP rare with glaucomatous damage
Prevalence of glaucoma at each IOP level
- Dose response relationship
- IOP 16-19
• risk > 2 times
- IOP > 23
• risk > 10 times
- In population IOP < 22 mmHg is More common than IOP > 22 mmHg
- risk of glaucoma with IOP <22 is approx 1/6 of patients with IOP >22 (2.8 compared to 12.8 see Baltimore Eye study table)
- however, 20 times more people have IOP <22 therefore, adjusted risk of glaucoma is 1:1
- 50% with glaucomatous damage have "normal" IOP
- IOP
- Is associated with nerve damage
- Is a risk factor for nerve damage - IOP is a causal risk factor
- Myopia is associated with POAG
- Myopia is a risk factor for POAG
- It is not a causal risk factor
|
|
- POAG in caucasians prevalence overall 1.7 - 2.1%,
- 0.5 - 1.0% age 40,
- rising to 4% age 70,
- 6% age 80 in whites,
- 12% age 70 in blacks
- In black populations higher incidence age 30-40 (4% St Lucia)
- Comparatively most angle closure in Chinese/Eskimo races
- 50% glaucoma in a community is undiagnosed
- Many patients never have functional visual loss
- but it can lead to blindness - responsible approximately 11% Australian and UK blind registrations
- Raised intraocular pressures
- "Normal" population mean 15.5 mmHg - Race - Afrocaribbean, African,
- Positive family history particularly in siblings
- Myopia
- ? Diabetes ? Hypertension
- Migraine/vasospasm for NTG
- Glaucoma is the commonest optic neuropathy
- Diagnosis is made when there is characteristic visual field changes which match the optic disc changes
- The intraocular pressure may be elevated or normal
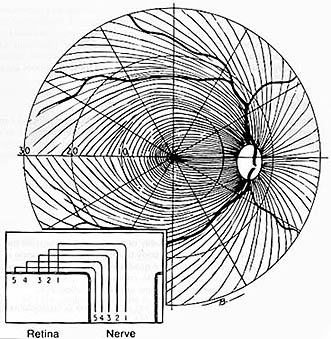
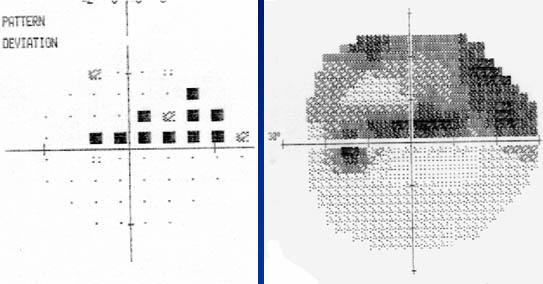
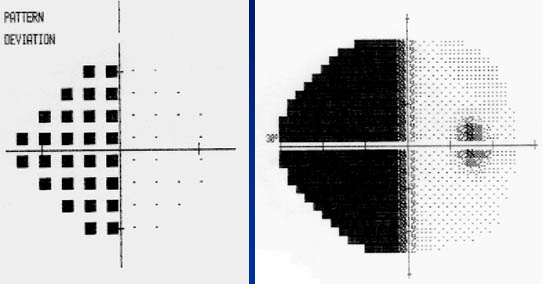
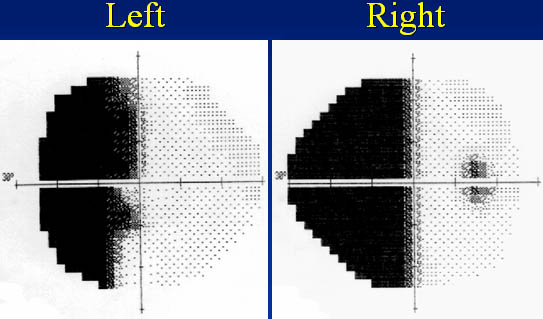
- generalised depression of field
- localised nerve fibre bundle defects/paracentral changes
- typical arcuate scotomata
- nasal step (central or peripheral), temporal sector defect
- advanced constriction (central and temporal island only)
- Not enlarged blind spot - as due to peripapillary atrophy
- In normal tension glaucoma field defects may be closer to fixation and steeper edge scotomas
- Defects often in superior field first
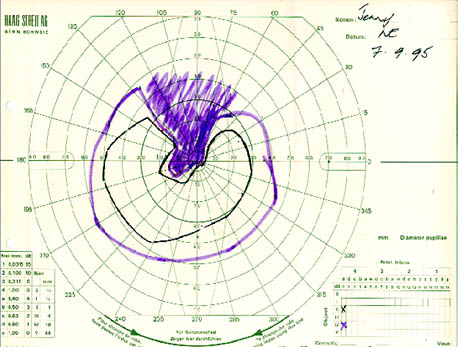
Goldmann field

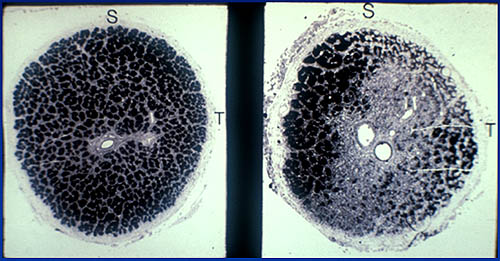
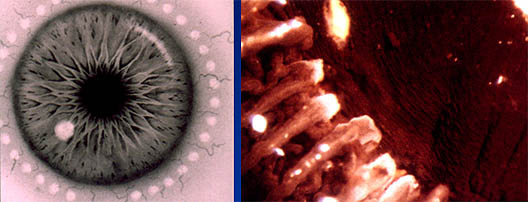
- Jonas - characteristic configuration of horizontally oval cup in vertically oval disc is normal.
- Rim with width greatest inferior > superior > nasal > temporal (ISNT rule)
- If not ? Glaucoma - Vertically oval cup
- Concentric enlargement of cup - if increase over time diagnostic
- Asymmetry of cups in both eyes > 0.2
- Focal loss of neuroretinal rim /notch / acquired pit
- Changes in vessels on optic disc: nasalisation, bayoneting, flyover vessels, focal narrowing of vessels, disc haemorrhage
- Peripapillary atrophy:
- Beta atrophy : increased in glaucoma, particularly where most neuroretinal rim loss - Nerve fibre layer changes:
- grooves, wedge defects, diffuse loss
- Disc changes may not be objective unless automated
- (new technology, eg. Heidelberg Retinal Tomograph, Nerve Fibre Layer Analyser) - Visual field progression:
- probability plots, mean deviation, pattern deviation, statpac (Beware short-term fluctuation)
- Progressor - Objective perimetry: Accumap
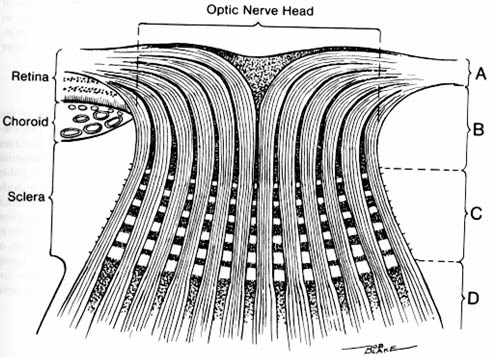
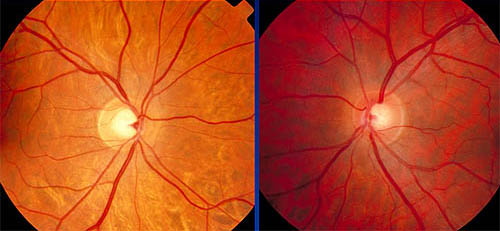
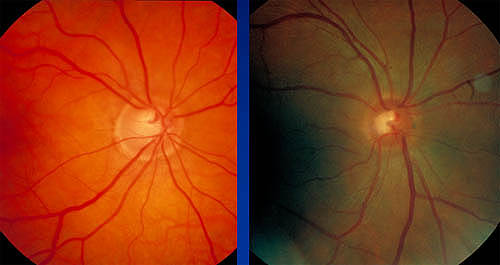


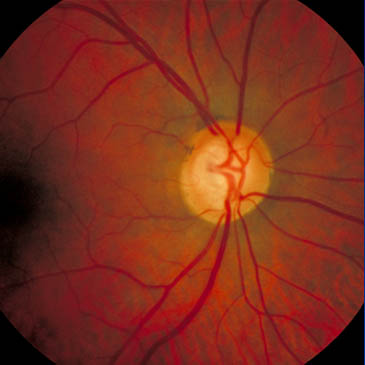

Superior disc margin Haemorrhage
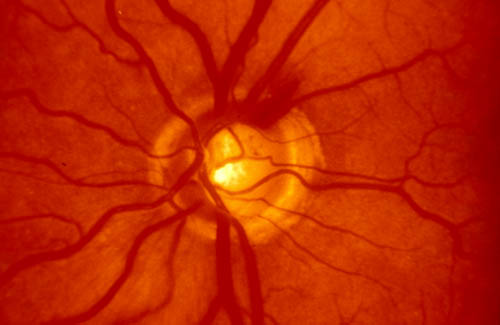
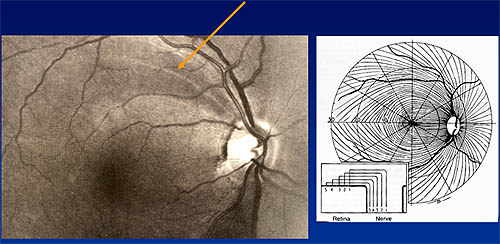
Note the nerve fibre layer arrangement and horizontal demarcation

Glaucoma Management
- repeat IOP measurement
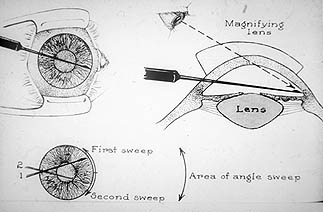
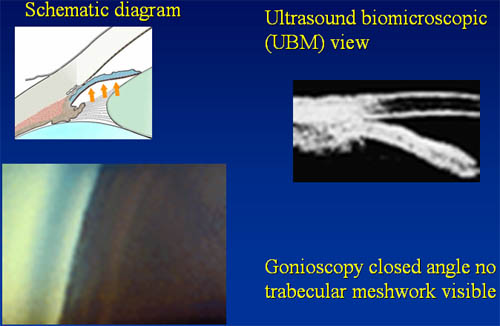
- Gonioscopy
- diurnal variation of IOP
- secondary glaucoma
- asymptomatic period
- good screening test
- test acceptable
- treatment available
- cost effective
- By general practitioner or optometrist.
- Recommendations:
- test IOP over 40 years of age, visual fields and disc examinations
- IOP tested by Goldmann applanation tonometry / Non-contact tonometry or Tonopen
- Optic disc assessment with stereoscopic lens at slit lamp
- Perimetry
- What level of IOP to use as cut off?
- 40 mmHG
- all will have glaucoma
- however, most will be missed
- valid clinical sign
- not necessarily a good screening test
- IOP is main causative risk currently known
- treatment aims to lower IOP
- select a target IOP which is safe for the individual's optic nerve
- Issues when not to treat
- non-compliant
- socio-economic
- Distance
- follow-up
- ? established glaucoma
-
Maximum medical treatment =
- minimum strength and number of drugs (within the combination) to achieve maximum reduction of IOP
- Estimate risk of damage
- Aim for target pressure not "normal" IOP
- existing optic disc damage
- existing visual field damage
- current baseline IOPs
- glaucoma risk factors (FHx, myopia etc)
- which agent to choose
- what concentration to choose
- unilateral vs bilateral
- how to instill drops
- Ocular hypertension/ POAG/Chronic ACG/Secondary glaucoma
- Reduce intraocular pressure to target
- Medical management initially - Monitor optic disc and field for progression
- No progression continue Rx
- If progression set lower target
• May need other intervention
- Statistical definition
- Not all develop glaucoma
- Higher IOP more likely to progress
- Treat generally over 30 mm Hg
- Medical
- Topical drops
- systemic medications
- Laser
- Argon Laser Trabeculoplasty
- Cyclodiode : Ciliary body ablation
- Surgery
- Trabeculectomy
- Non-penetrating surgery
- Drainage tubes
Medical Treatment
- high concentration of drug in one drop
- avoid systemic side effects
- punctal occlusion
- no blinking
- use only one drop
|
- Reduce aqueous production |
- Action
- Increases uveoscleral outflow via prostaglandin receptors in angle and ciliary muscle.
- Alters ground substance in ciliary body - Agents
- Latanoprost (Xalatan) Nocte
- Travaprost (Travatan) Nocte
- Bimatoprost (Lumigan) Nocte - Side Effects
- Increased iris pigmentation in hazel eyes
- Increased lash growth and pigmentation
- Possibility uveitis
- Cystoid macular oedema - aphakia
- No systemic side effects
- Action
- Beta 2 mediated binding to nonpigmented ciliary epithelium, changes intracellular adenylate cyclase activity and CAMP production which reduces aqueous production - Agents (all used topically)
- Timolol 0.25%, 0.5% (bd)
- Betaxolol 0.25%, 0.5% (Beta 1 selective) (bd)
- Levobunolol 0.25%, 0.5% (bd) - Side effects
- significant systemic absorption
- broncho-constriction, bradycardia, CNS effects
- Action
- initial vasoconstriction of ciliary blood vessels (alpha 1 mediated). Longterm by increased facility of outflow via both conventional and uveoscleral pathways - Agents
- Dipivefrine (propine) 0.1% (bd)
• pro-drug absorbed by cornea and converted into active drug (adrenaline) by corneal esterases - Side effects
- Local: red eye due to blepharoconjunctivitis, or follicular conjunctivitis
- Systemic: rarely seen (hypertension, angina)
- Action
- initial vasoconstriction of ciliary blood vessels. Longterm by increased facility of outflow via both conventional and uveoscleral pathways - Agents
- Brimonidine (Alphagan)
- Apraclonidine (Iopidine)
• Tachyphalaxis after 6 weeks use
• Uses: Post laser IOP spikes - Side effects
- Local: red eye due to blepharoconjunctivitis, or follicular conjunctivitis
- Systemic: Sedation in children Dry mouth, Headache,Fatigue, Palpitations
- Action
- contract ciliary muscle opening the trabecular meshwork and increasing facility of outflow - Direct acting - parasympathomimetic agents
- Pilocarpine 0.5%, 1%, 2%, 4%, 6% (qid)
- Carbachol 1.5%, 3% 9 (tds) - Indirect acting - cholinesterase inhibitors
- Phospholine iodide 0.03%, 0.06%, 0.125%, 0.25% (bd) - Side effects
- Local: redness and stinging, toxic papillary conjunctivitis, miosis, headaches
- Systemic: bradycardia, flushing
- Action
- suppress aqueous production by inhibition of carbonic anhydrase in ciliary epithelium - Agents (oral or IVI, topical agent being released)
- Diamox (acetazolamide) 250 mg up to qid - Darinide (dichlorphenamide) 50 mg up to tds - Side effects
- Paraesthesias
- Malaise
- Metabolic acidosis
- Hypokalemia
- Gastrointestinal upset
- Renal stones
- Sulphur compound therefore check allergy status
- Action
- suppress aqueous production by inhibition of carbonic anhydrase in ciliary epithelium - Agents
- Dorzolamide (Trusopt) bd to tds dose
- Brinzolamide (Azopt) bd - Side effects
- Minimal systemic side effects
- Timpilo
- Timolol 0.5% with pilocarpine 2% or 4% - Cosopt
- Timolol 0.5% with dorzolamide - Xalacom
- Timolol 0.5% with latanoprost
|

|
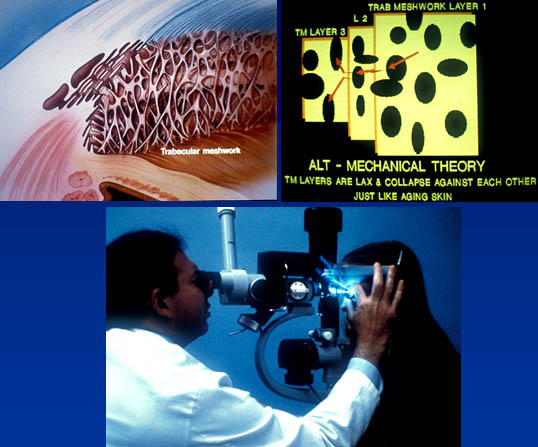
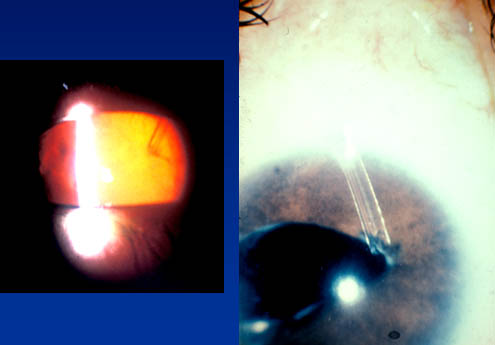
Laser therapy in Glaucoma
- Initially used to induce glaucoma in animal models
- Treat trabecular meshwork 180-360 degrees - More effective on pigmented meshwork
- Pigment dispersion/pseudoexfoliation/elderly
- Increases outflow
- Opens channels in meshwork and alter cell profile
- Mechanism of Action
- Mechanical
• contraction of scar tissue pulls inter-trabecular spaces open- Metabolic
• Laser burn increases phagocytic activity of trabecular meshwork endothelium
- More frequently used in Australia /USA than UK
- Long term escape
- 50% fail at 5 years - Side effects
- IOP spike, uveitis, haemorrhage, corneal burns, pain, PAS - Can lower IOP 30%
- Treat ciliary body through sclera
- Requires local anaesthetic block
- Used in refractory glaucoma
- Lowers IOP mean 50%
- Requires retreatment in 2/3 over 18 months
- Side effects
- Hypotony, uveitis, reduced VA, conjunctival burn
Glaucoma Surgery
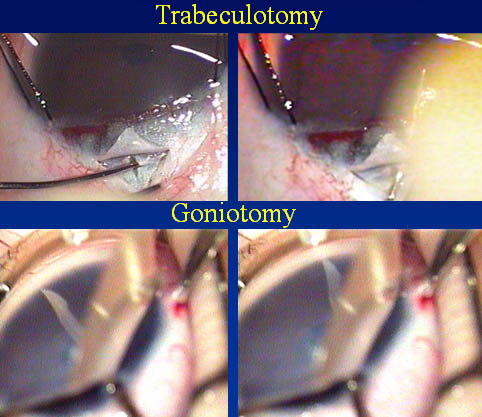
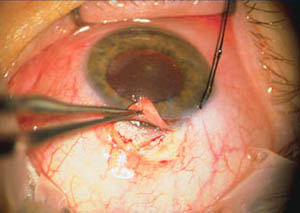
- Trabeculectomy
- Enhanced with anti-metabolites
• 5 Fluouracil, Mitomycin C, Strontium 90 - Non-penetrating
- Viscocanalostomy/deep sclerectomy - Drainage tubes
- Molteno/Ahmed/Baerveldt
|
|
|
|
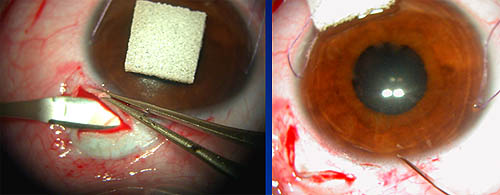

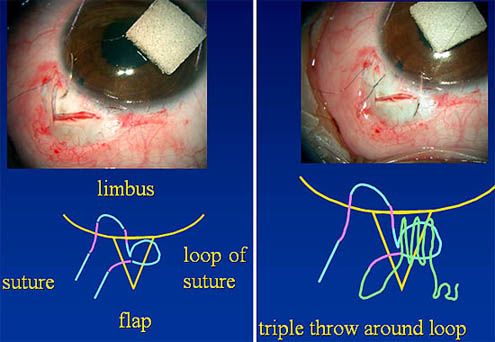
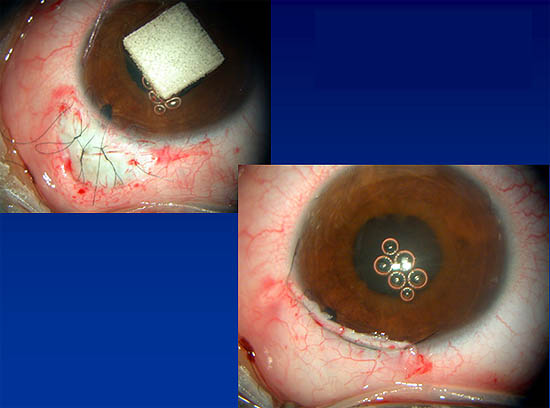
- Success up to 90% but some long-term failure
- Mean IOP achieved 17 mm Hg
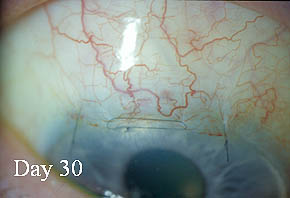
- Recent changes
- Size of surgical site
- Releasable sutures/argon laser suture-lysis
- Enhanced with antimetabolites where risk of failure
• Youth, previous surgery, AfroCarribean, topical medications, rubeosis, uveitis, diabetes etc
|
|
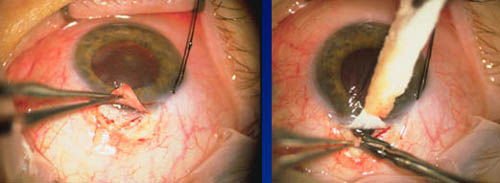
- Usually if Trabeculectomy fails
- Tube into anterior chamber, plate at equator
- Success up to 80% at 3 years
- Complications more severe than trabeculectomy
- Particularly in children - Can obstruct or erode and be exposed
- Normal Tension Glaucoma
- 24 hour ambulatory Bp monitoring
- Treatment vasospasm ? Ca channel blockers
- Carotid artery investigation
- Cardiology opinion - Exclude intracranial pathology
- CT Scan if disc and field don't fit
- Late presentation
- Advanced disease
- Young at presentation
- Inadequate treatment
- Poor compliance
- Compliance
- Side effects medications
- Holistic approach
- Lifelong condition
- Establish partnership
|
|
|
|
-
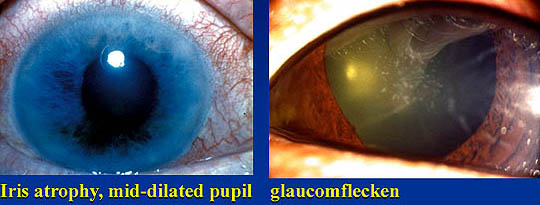
1. Acetazolamide (250-500 mg) IV stat. then 125 to 250 mg qid P.O. until symptoms subside.
2. Topical pilocarpine 4% stat., then qid
3. Analgesics and antiemetics as required.
4. Topical b-blocker stat., then bd thereafter.
5. Topical alfa2-agonist stat., then bd regularly.
6. Topical steroids (prednisolone acetate, 1% qid).
Contra-indications and hypersensitivity to drugs should be excluded prior to starting treatment
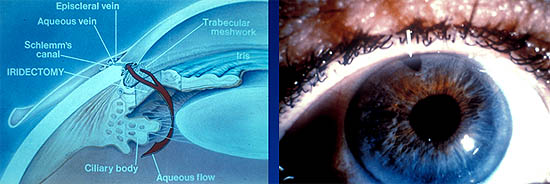
Laser iridotomy is the definitive method of managing PAC due to pupil-block, the major mechanism in 85-90% of cases
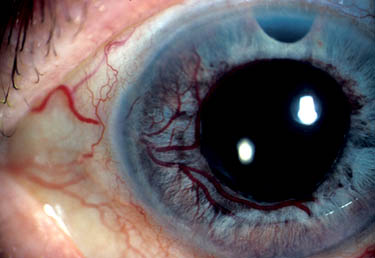
- SECONDARY OPEN ANGLE GLAUCOMAS
- Outflow resistance pre-trabecular
• Epithelialisation of the chamber angle
• Endothelialisation of the chamber angle (early ICE-Syndrome)
• Neovascular glaucoma stage 2- Outflow resistance trabecular
• Pigmentary glaucoma
• Capsular glaucoma
• Steroid induced glaucoma
• Inflammatory glaucoma
• Phacolitic glaucoma
• Posner-Schlossman-Syndrome
• Heterochromie cyclitis Fuchs
• Ghost-cell-Glaucoma
• Haemolytic Glaucoma (after anterior chamber bleeding)
• Neurofibromatosis
• Siderosis
• Posttraumatic glaucoma with angle recession- Outflow resistance post-trabecular
• Episcleral Glaucoma (Sturge-Weber-Syndrome; arteriovenous fistulas, idiopathic)
-
- Anterior type: outflow resistance in chamber angle
• Neovascular glaucoma stage 3
• Glaucoma in progressed Irido-Corneo-Endothelial-Syndrome (ICE-Syndrome)
- Posterior type with pupillary block and vitreociliary block mechanism
• Glaucoma with pupillary block due to synechias
• Dislocation of the lens, traumatic
• Microspherophakia in Weill-Marchesani-Syndrome (Ectopia lentis); Cataracta intumescens
• Iridoschisis
- Posterior type with anterior displacement of Iris-Lens-Diaphragm
• Glaucoma in association with choroidal bleeding, oedema of ciliary body, ciliary body cysts, tumors (malignant melanoma, leiomyoma);
• Gaucoma associated with contraction of retrolental tissue (persistent hyperplasic primary vitreous PHPV; premature retinopathy)

- Incidence 1: 10,000 births
- Suspicion of congenital glaucoma requires immediate referral to an ophthalmologist
|
|

|
|
|
|
|