John Grigg
Senior Lecturer
Department of Ophthalmology, University of Sydney
[email protected]
- Note the dimensions of the globe, the lens, The medial recti are easily visualised. The right optic nerve (screen left) is shown extending to the optic canal. Note the close proximity to the ethmoid sinuses. Note the thickness of the lateral orbital walls.
Learning Topics
- What role does the bony orbit play?
- What are the ocular complications of the thin ethmoidal sinus bony walls?


Clinical Description
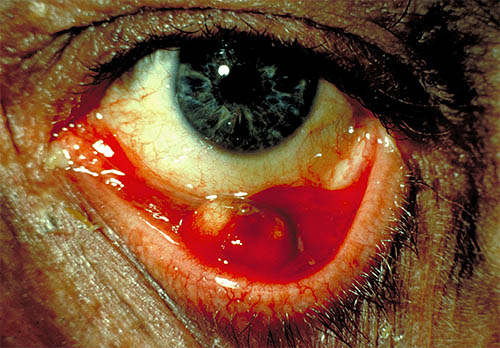
- Grossly proptotic right eye. This is chemosis of the conjunctiva.
Learning Topics
- What are 2 ocular components that may be affected by proptosis?
- How may proptosis cause visual loss?

Note prominent left globe (proptosis) in this photo taken from above in a patient with thyroid eye disease

Clinical Description
- Axial proptosis due to optic nerve glioma. The glioma is within the muscle cone and so pushes the globe straight forward.
Learning Topics
- What orbital structures when enlarged will produce axial proptosis?
- What are 2 conditions that may cause axial proptosis?

Clinical Description
- Note the eyelid retraction with excessive scleral 'show' superiorly. This patient is trying to look up but is unable to. Thyroid eye disease is an autoimmune disorder which affects primarily ocular muscles and orbital contents, particularly the orbital fat.
Learning Topics
- How may vision be lost in Thyroid eye disease?


Clinical Description
- Note the closed eye with swelling in both eyelids and erythema particularly the upper lid. This is the commonest reason for an ophthalmic admission to hospital. The infection usually starts with swelling and redness of the eyelids. At this stage the infection is in front of the orbital septum and classified as pre-septal orbital cellulitis. Once the infection progresses behind the septum the conjunctiva can become red and oedematous, eye movements can be limited and proptosis can occur. When post-septal orbital cellulitis occurs the vision is threatened.
Learning Topics
- From your knowledge of orbital anatomy where is the likely source of infection in non-traumatic cases.
- In the paediatric age group what are 3 likely organisms causing this condition.
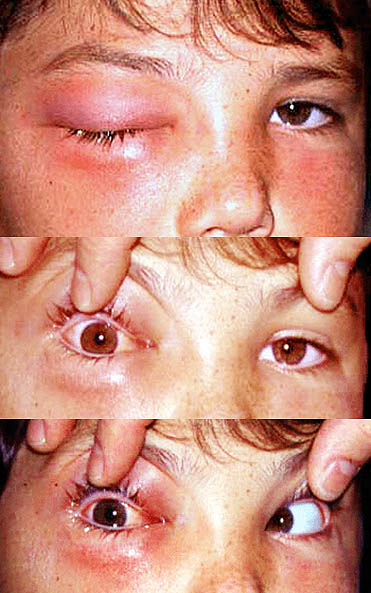
In this child note the restriction in eye movement indicating orbital involvement with the infection.

Clinical Description
- There is partial right ptosis and right miosis (small pupil).
Learning Topics
- What is the course of the sympathetic nerve supply to the eye?
- What are 3 possible causes for Right Horner's syndrome?

Clinical Description
- Left lower lid bruising with limitation of elevation. The orbital floor and the medial wall are the thinnest and thus the weakest of the orbital walls. A blow to the orbit causes the bone to buckle out resulting in fracture. The main complication is the entrapment of orbital contents in the fracture which then limits eye movement.
Learning Topics
- Why may the patient complain of upper lip paraesthesia with an orbital blow out fracture?

Clinical Description
- These are excess folds in the medial aspect of the eyelids. They are very common in infants and Asian race.

Clinical Description
- Notched defects are seen in the upper lid. The white opacity on the inferior cornea is a limbal dermoid. This constellation of clinical signs can be seen in Goldenhar's syndrome.
Learning Topics
- What is the function of the eyelids?
- What problems might this patient have?

Clinical Description
- Minor swelling of the right upper and lower eyelids. Note the loss of facial wrinkles on the right. The skin covering the eyelids is very thin and easily distensible for these reasons it may be affected by dermatitis following exposure to environmental allergens.
Learning Topics
- How are the allergens commonly transmitted to the eyelids?

Clinical Description
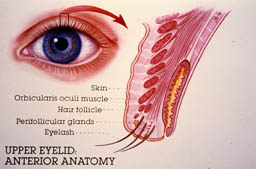


- An inflamed swelling in the lid margin pointing externally. Pathology is an acute infection of a lash follicle and its associated gland of Zeis. Staphylococcus is the common agent. Most resolve spontaneously or with removal of the lash and hot compresses.
Clinical Description
- This is an acute infection of a meibomian gland. This is a swelling within the tarsal plate. The treatment is hot compresses but some cases require surgical incision.

Clinical Description
- A Chronic obstruction to a meibomian gland resulting in inflammation in the surrounding tissues.

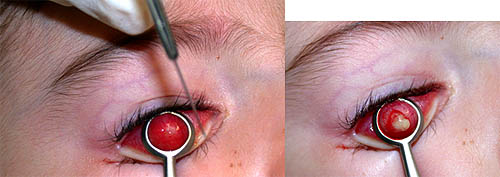
Lower images: Chalazion in a child and incision with release of lipid material
Clinical Description
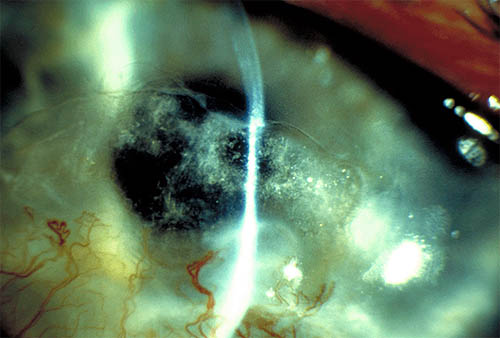
- Pigmented conjunctival lesion that is freely mobile in the conjunctiva. The lesions are usually pigmented but they may also be non-pigmented.
Learning Topics
- What features would make you suspect a malignant tumour instead?
- From your knowledge of pathology in what layer would the naevus cells found?

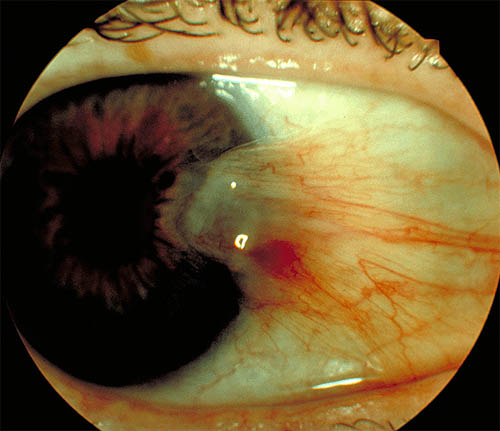
Clinical Description
- Note the deeply pigmented lesion that is primarily located on the tarsal conjunctiva. Pigmented lesions that occur on the tarsal conjunctiva and the fornices are more likely to be malignant.
Learning Topics
- How is the melanoma differentiated from a benign lesion clinically?

Clinical Description
- Note the yellow area on the cornea stained by fluorescein. The unaffected area of the cornea does
not show any yellow fluorescence indicating that the fluorescein is not binding to the epithelial basement membrane.
Learning Topics
- What different pathology is highlighted by Rose Bengal staining compared to Fluorescein staining?
- What light source do you select to make the fluorescein fluoresce?

Clinical Description
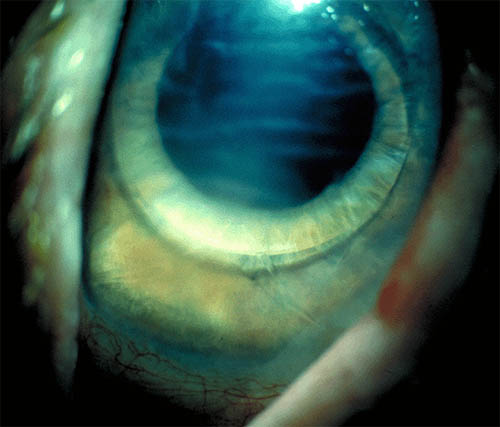
- Note the slight cloudiness of the cornea and the presence of folds in the cornea at the level of descemets membrane. The commonest acute cause of stromal oedema is postoperatively (although smaller wound incisions reduce the incidence), which usually resolves over several weeks. Infections are another common cause of stromal oedema. Chronic causes of corneal oedema occur when there is a reduction or function of the corneal endothelial cells.
Learning Topics
- How do you decide if the cornea is oedematous compared to the other eye?
Clinical Description
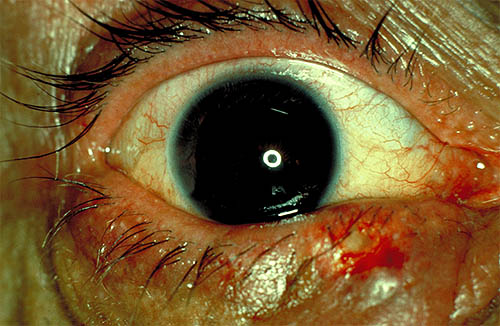
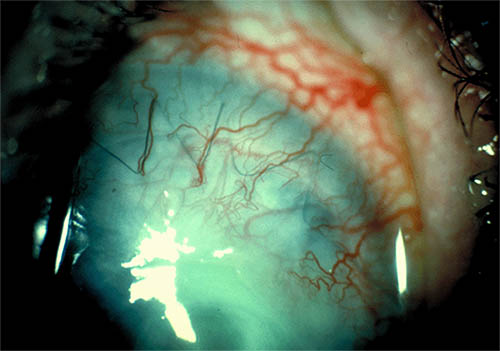
- Small blood vessels extend onto the cornea beyond the limit of the normal limbal vascular arcade. These vessels remain superficial at the level of the epithelial-stromal junction. The stimulus for this vessel growth is due to mild chronic inflammation which may be infective, hypoxic or mechanical. Contact lens wear is a common cause usually not as extensive as shown in this slide.
Learning Topics
- What keeps the cornea clear?
- Why aren't there any blood vessels in the cornea normally?
- How does the cornea get its nutrients? And oxygen?
Clinical Description
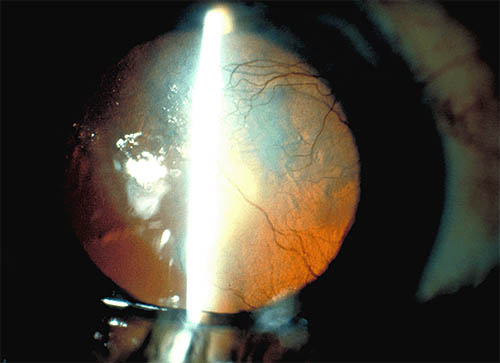
- Corneal retro-illumination photo highlighting the vessels crossing the cornea including the visual axis. The stimulus for this vessel growth is due to severe chronic inflammation which may be infective, hypoxic or mechanical.
Learning Topics
- When the inflammatory stimulus is removed then blood gradually ceases to flow and the vessels collapse leaving thin white cords/lines. These are called ghost vessels.
Clinical Description
- Chronic inflammation will result in vascularisation of the cornea and lipid deposition. The most common cause for this is HSV infection.
Learning Topics
- A winged shaped growth of tissue over the surface of the cornea.
Learning Topics
- Contributing factors to development of a pterygium are sunlight irritating environment (such as dust or grit) and family history
- Treatment involves ocular lubricants
- Affects vision by causing distortion of the cornea (astigmatism) and if advanced may intrude onto visual axis
- Treatment is by excision
Clinical Description