-
Dr Ivan Ho
Sydney Eye Hospital
- 110 million people with DM worldwide in 1994
- Projected incidence in 2010 is 221 million worldwide per year
- Prevalence of DM in general population is ~3-4%
- 110 million people with DM worldwide in 1994
- Projected incidence in 2010 is 221 million worldwide per year
- Prevalence of DM in general population is ~3-4%
- Leading cause of blindness in patients aged 20-64 years in developed nations
- After 20 years of DM, 99% of type 1 and 60% of type 2 have some retinopathy
- Exact mechanisms leading to development of DR are not understood
- Thickening of capillary basement membrane
- Loss of capillary mural pericytes
- Basement membrane hypertrophy and endothelial cell loss
- Breakdown of blood-retinal barrier
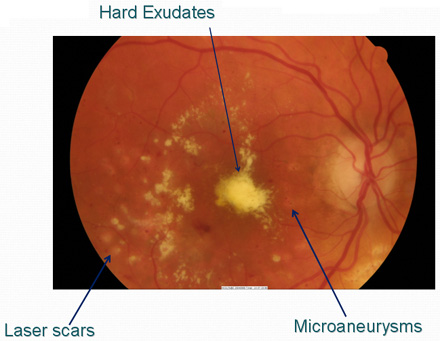
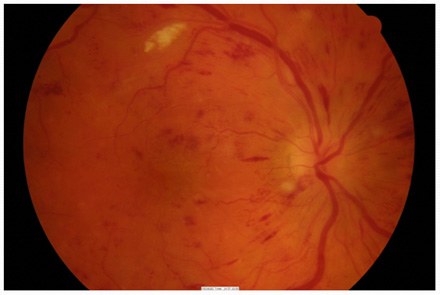
- Earliest clinical sign of DR is presence of microaneurysms
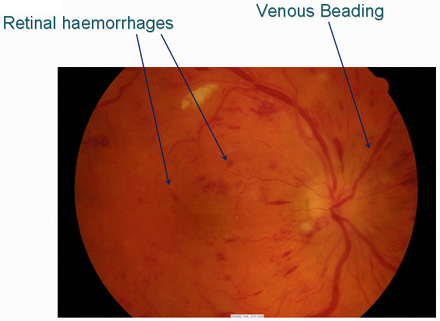
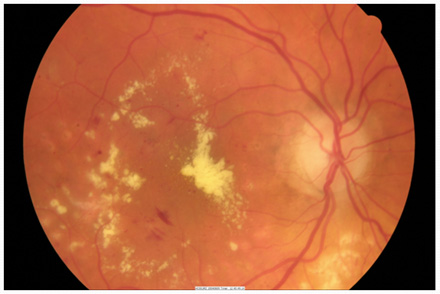
- Retinal ischaemia → lipid exudation, haemorrhage and release of pro-angiogenic factors
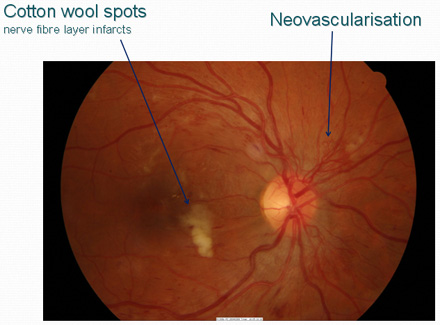
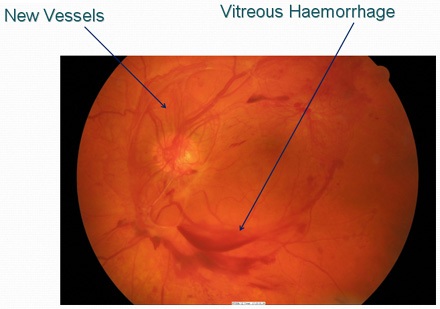
- Neovascularisation → haemorrhage → fibrosis and traction detachment
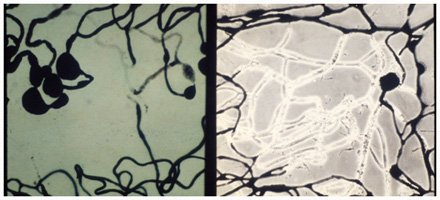
Left: Blood vessels show tortuosity and microaneurysm formation
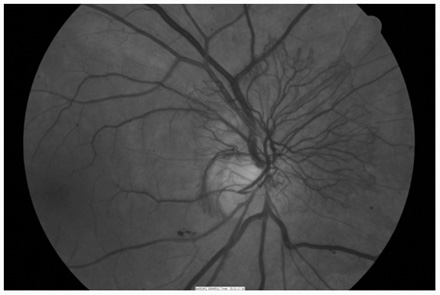
Right: Capillary closure on phase microscopy
- Capillary microaneurysm associated with an area of hemorrhage
- Cotton-wool spot: Precapillary arteriole occlusion causing microinfarction of the nerve fiber layer

- Duration of diabetes
Key factor in DR development - Control of diabetes
Key factor in DR progression - HT, Smoking, Cholesterol
Key modifiable factor in DR progression
- Age
- Type of diabetes
- Renal disease
- Pregnancy
- Atherosclerotic disease
- Medication
- By 5 years, 25% have some DR
- By 10 years, 60% have some DR
- By 15 years, 80% have some DR
• 25% have PDR at 15 years
- By 5 years, there is some DR present in
• 40% of patients on insulin
• 24% of patients not taking insulin
• 2% of patients have PDR - By 19 years, some DR is present in
• 84% of patients on insulin
• 53% of patients not taking insulin
• 25% of patients have PDR

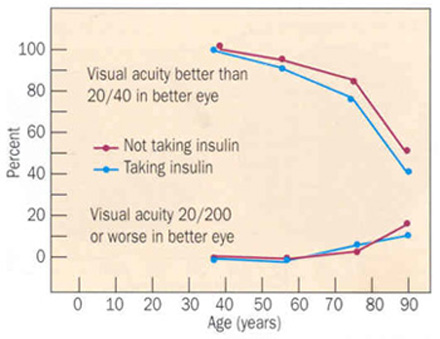
No visual impairment vs legal blindness in all diabetics diagnosed after age 30 years
- Primarily caused by complications of the microvascular abnormalities
-
• Vitreous hemorrhage (VH)
• Macular edema (CSME)
• Tractional retinal detachment (TRD)
• Neovascular glaucoma (NVG)
• Macular ischemia
- 90% of severe vision loss can be avoided with treatment1
- In one study of 2000 patients2
-
• 11% of type 1 with high-risk PDR had not been seen by an ophthalmologist in 2 years
• 7% of type 2 with high-risk PDR also had not been seen in 2 years
• 46% of eyes with high-risk PDR had not received laser photocoagulation
2. Klein R. et al., Ophthalmology 1987
- Control BSL (HbA1c <8%), BP, cholesterol, weight etc
- Get GP, Endocrinologist, Physicians involved
- Ophthalmologist
-
• Laser treatment
• Intravitreal injections (steroids, anti-VEGF agents)
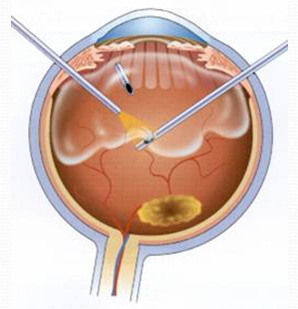
• Surgery
• Regular eye review for early detection of retinopathy
- Discomfort
- Transient visual blur
- Peripheral field loss
- Glare sensitivity
- Colour discrimination
- Long term visual loss (from worsening maculopathy, foveal burn)
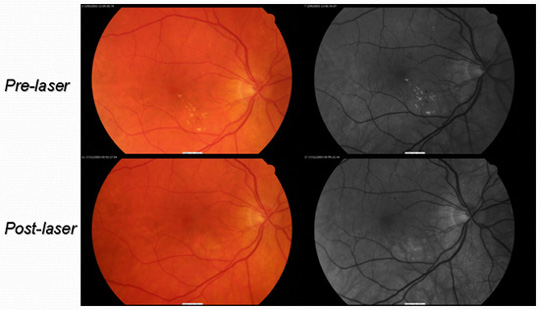
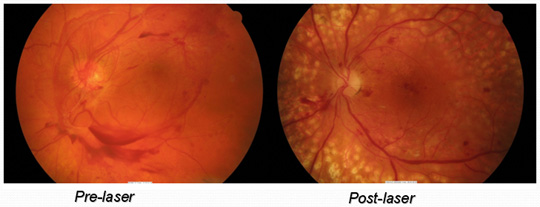
For macular oedema or neovascularisation
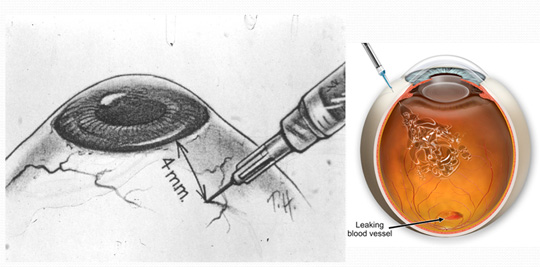
For vitreous haemorrhage, tractional retinal detachment or macular fibrosis
- Strict control of BSL and other risks is imperative
- Team approach with GP, endocrinologist, others
- Early detection of any retinopathy through regular examination