-
Dr Ivan Ho
Sydney Eye Hospital
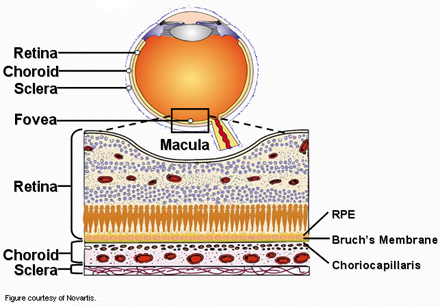
- Age related wearing to the back of the eye
- Two types:
- Dry (non-neovascular) 90% of ARMD cases
= slow, progressive decline in central visual function- Wet (neovascular) 10%
= rapid, more substantial loss of vision
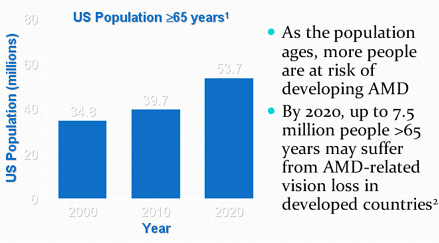
1. US Census Bureau population estimates.
Available at: http://eire.census.gov/popes/estimates.php.
Accessed March 10, 2004.
2. Hyman L. In: Hampton GR, Nelson PT, eds.
Age-Related Macular Degeneration: Principles and Practice.
Raven Press; 1992.
- Several risk factors, other than age, have been suggested:
-
• Family history
• Gender - female
• Race - white
• Smoking
• Genetic factors - genes for complement factors
• High cholesterol
• Hypertension and cardiovascular disease
• Low intake of antioxidants/lutein
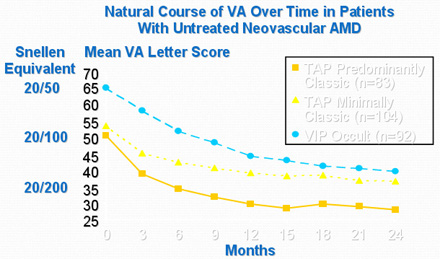
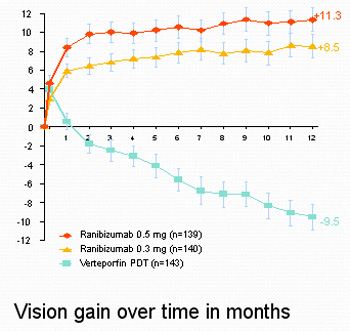
TAP = Treatment of ARMD With Photodynamic Therapy Study;
VA = visual acuity;
VIP = Verteporfin in Photodynamic Therapy Study.
*TAP and VIP placebo groups.
Data on file, Novartis.
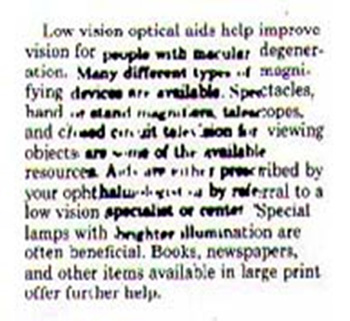
- More likely to have difficulty with daily activities such as meal preparation, handling money, and using the telephone1
- Increased risk of recurrent falls2
- Experience more depression and emotional distress than those without AMD3
- Potentially as debilitating as other chronic disabling diseases, such as arthritis, COPD, and AIDS
AIDS = acquired immune deficiency syndrome;
COPD = chronic obstructive pulmonary disease.
1. Williams RA et al. Arch Ophthalmol. 1998;116:514-520.
2. Ivers RQ et al. J Am Geriatr Soc. 1998;46:58-64.
3. Brody BL et al. Ophthalmology. 2001;108:1893-1901.
- Reduced central visual acuity
- Central scotoma
- Metamorphopsia
- Decreased contrast sensitivity
- Decreased color vision

Reprinted with permission from Bressler NM. J Am Board Fam Pract. 2002;15:142-152.
- Patients with neovascular AMD may have difficulty with visual tasks
-
• Reading
• Telling the time
• Recognizing facial expressions
• Driving
Bressler NM. J Am Board Fam Pract. 2002;15:142-152.
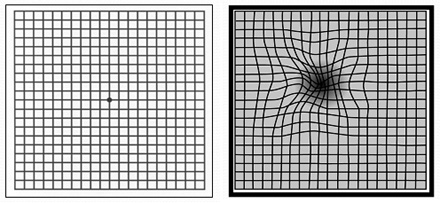
- Amsler grids can facilitate early detection
- Can be done by patient at home
- Signs suggestive of neovascular AMD include
-
• Distortion
• Blurring
• Darkening or discoloration of the grid lines
• Inability to fixate on the central dot
1. Fine SL. Ophthalmology. 1985;92:603-609
2. Oshinskie LJ. In: Jennings BJ, ed. Optom Clin. 1996;5:25-53
3. Mattice E, Wolfe CP. J Ophthalmic Nurs Technol. 1986;5:34
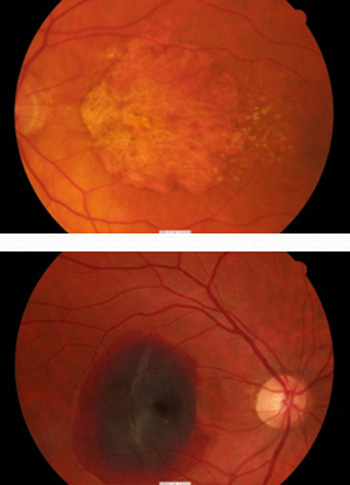
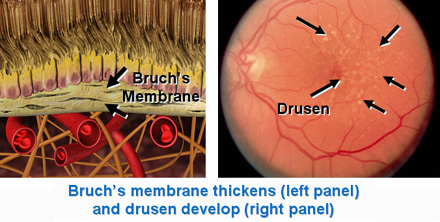
- Patients are usually asymptomatic and do not experience vision loss 1
- Examination reveals several small drusen or a few medium-sized drusen 2
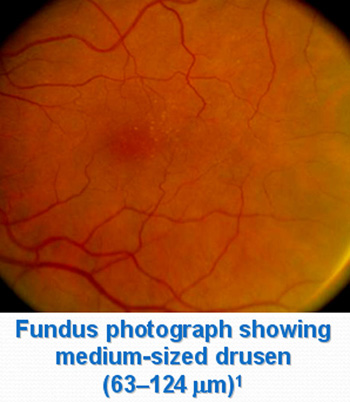
Photo reprinted with permission from Age-Related Eye Disease Study Research Group. Arch Ophthalmol. 2001;119:1417-1436
1. Age-Related Eye Disease Study Research Group. Arch Ophthalmol. 2001;119:1417-1436
2. National Eye Institute website. Available at: www.nei.nih.gov/health/maculardegen/armd_facts.htm. Accessed December 17, 2003
- Examination reveals many medium-sized drusen or ≥1 large drusen 1, 2
- Vision may be impaired 2
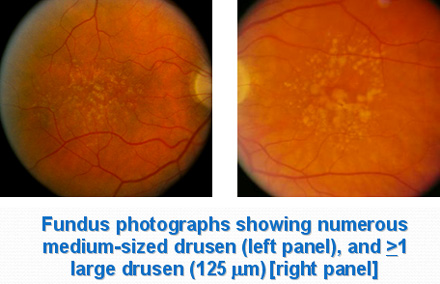
Photo, left, courtesy of Novartis. Photo, right, reprinted with permission from Age-Related Eye Disease Study Research Group. Arch Ophthalmol. 2001;119:1417-1436
1. Age-Related Eye Disease Study Research Group. Arch Ophthalmol. 2001;119:1417-1436
2. National Eye Institute Web site. Available at: www.nei.nih.gov/health/maculardegen/armd_facts.htm. Accessed December 17, 2003
- Vision impairment is more severe 1
-
• May have difficulty recognizing faces from a distance
- Examination reveals 2
-
• Presence of drusen
• Degeneration of RPE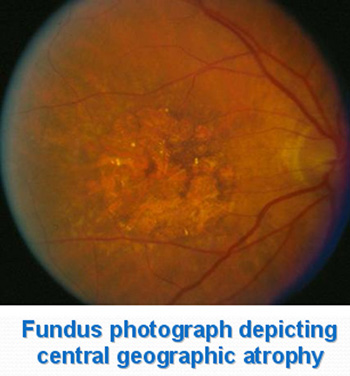
Photo courtesy of Novartis
1. National Eye Institute Web site. Available at: www.nei.nih.gov/health/maculardegen/armd_facts.htm. Accessed December 17, 2003
2. Data on file, Novartis
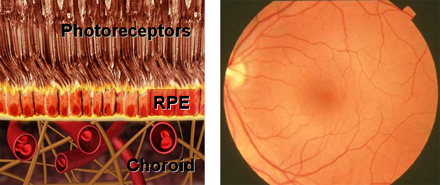
Photos courtesy of Novartis
Photos courtesy of Novartis
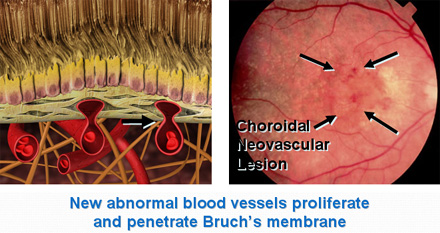
Photos courtesy of Novartis
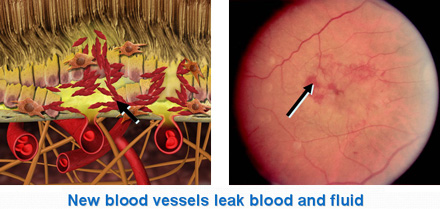
Photos courtesy of Novartis
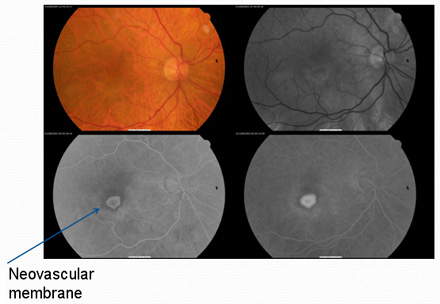
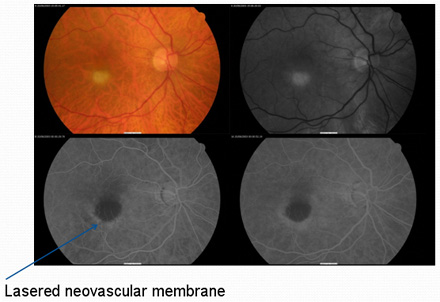
Fluorescein angiography enables visualization of neovascular lesions
- Fluorescein does not penetrate healthy RPE and retinal capillaries
- Type, size, and location of CNV can be determined 1
- Neovascular and non-neovascular AMD can be distinguished 2
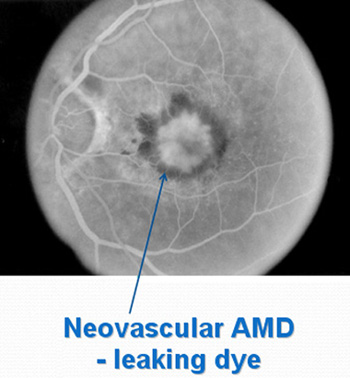
Photos courtesy of Novartis
1. Bressler NM. J Am Board Fam Pract. 2002;15;142-152
2. Data on file, Novartis
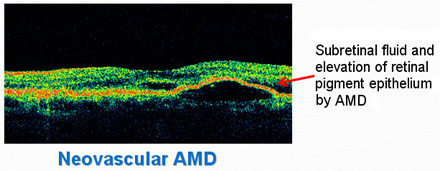
OCT enables pseudo-histological cross-section of retina in-vivo
Non-neovascular (dry) AMD
- There is no commonly accepted treatment found to reverse the effects of the non-neovascular form of AMD1
- Treatment may delay and possibly prevent intermediate non-neovascular AMD from progressing to the advanced stage2
-
• High levels of zinc and antioxidants may play a role in slowing the progression of advanced AMD (AREDS study)3
1. Oshinskie LJ. In: Jennings BJ, ed. Optom Clin. 1996;5:25-53
2. National Eye Institute Web site. Available at: www.nei.nih.gov/health/maculardegen/armd_facts.htm. Accessed December 17, 2003
3. Age-Related Eye Disease Study Research Group. Arch Ophthalmol. 2001;119:1417-1436
Results from AREDS1,2
Estimate of Risk Reduction in Developing Any Advanced AMD*: Intermediate AMD or Monocular Advanced AMD
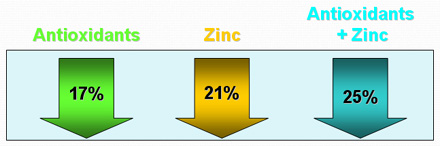
*Over the duration of the study (mean 6.3 years)
1. Age-Related Eye Disease Study Research Group. Arch Ophthalmol. 2001;119:1417-1436
2. Sackett CS, Schenning S. Insight. 2002;27:5-7
- Stop smoking
- Exercise
- Dark green, leafy vegetable
- Colourful fruits and vegetables
- Tree-nuts
- Fish or Omega-3 supplements
- Margarine and butter in moderation
- Laser photocoagulation - AMD away from fovea
- Visudyne® therapy - certain subset of neovascular AMD
- Retinal surgery - limited indications today
- Anti-VEGF agents (Lucentis, Avastin) - current gold standard
- Gene therapy - experimental
- Two-step process
-
• IV administration of a light-activated drug (Visudyne)
• Drug activation by administration of a specific wavelength of light delivered with a nonthermal laser
- Results in targeted occlusion of vessels within CNV, which preserves overlying retinal tissue
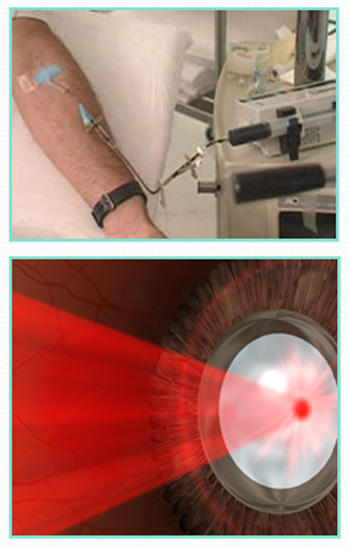
Photos courtesy of Novartis
Schmidt-Erfurth U, Hasan T. Surv Ophthalmol. 2000;45:195-214
Current indications:
- Intravitreal gas displacement of large submacular haemorrhage
- Subretinal removal of neovascular membrane in selected cases (non-subfoveal)
- Retinal Translocation/Rotation - very limited indication
- Retinal stem-cell transplant (experimental)
Current indications:
- Vascular Endothelial Growth Factor involved in:
-
• Vascular permeability
• Vascular formation - Anti-VEGF agents (Lucentis or Avastin) blocks all forms of VEGF reducing vascular leakage and growth
- Current gold-standard in treatment of neovascular AMD - monthly intravitreal injection for 2 years
Lucentis is the only treatment that results in an improvement and maintence of vision in neovascular AMD
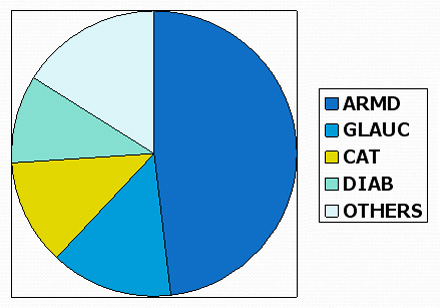
- AMD is the leading cause of blindness in western aging population
- AMD has multifactorial risk factors/cause
- Many exciting emerging treatment for neovascular AMD but no effective treatment for non-neovascular AMD to date
- Early detection important for best treatment result